|
Read time: 9 min
|
Posted on:
Read time: 9 min
Posted on:




Antibiotics are medications commonly prescribed to treat bacterial infections. There are hundreds of different antibiotics, but what is meant when one of them is called broad-spectrum?
Broad-spectrum antibiotics are medications that treat a broad range of bacteria, not just one strain. This makes them helpful for treating infections from multiple bacterial strains, which means they can be quickly prescribed without a doctor needing to confirm the type of bacteria causing the infection.
However, there are some risks associated with broad-spectrum antibiotics, such as a greater risk of side effects or antibacterial resistance. In this article, we will provide examples of broad-spectrum antibiotics, discuss what separates broad-spectrum from narrow-spectrum antibiotics, and outline the pros and cons of these antibiotics.
Antibiotics are a type of medication used to treat bacterial infections. They accomplish this through different mechanisms, with some antibiotics killing the bacteria directly and others interfering with their ability to grow and reproduce. For example, some antibiotics prevent bacteria from creating specific proteins, making their cell walls weak or incomplete.
Some of the bacterial infections that antibiotics may be prescribed to treat include:
However, not all bacterial infections require antibiotics. For example, even when caused by a bacterial infection, ear infections and sinus infections may not need antibiotics as the body’s immune system is often enough to clear the infection.
Most notably, antibiotics are only intended to treat bacterial infections. Taking them when you have a viral infection will not only leave the infection untreated, but can also cause unpleasant side effects and weaken your immune system, resulting in a longer or more severe infection. Knowing the consequences of incorrect antibiotic use, most antibiotics, besides some topical creams, can only be obtained with a prescription from your doctor, as they can ensure that you’re taking an antibiotic only when needed.
Antibiotics are available in many formats, including pills, liquid suspensions, topical creams or sprays, and IV infusions. The form an antibiotic is prescribed will depend on the type and severity of the infection. For example, ointments are prescribed for skin infections, whereas a hospital may start a patient on an antibiotic IV infusion in cases of sepsis.
Antibiotics also fall into different classes, grouped according to their chemical structure and the pharmacological effect they exhibit on bacteria. This means that drugs within a class often treat similar bacteria.
Some antibiotic classes include:
In addition to being separated by classes, other terms used to categorize antibiotics include broad-spectrum or narrow-spectrum, which refers to the number of bacterial strains they are effective against.
Broad-spectrum antibiotics refer to a class of antibiotics that target both gram-positive and gram-negative bacterial groups, which means they are effective against a large range of disease-causing bacteria. Gram-positive bacteria have a single thick cell wall surrounding them, whereas the cell wall of gram-negative bacteria is much smaller, but they also have an outer membrane.
The structural differences between these two types of bacteria means that the way an antibiotic works may be effective against one but not the other. However, with broad-spectrum antibiotics, they are effective against both.
Some of the classes of antibiotics that are considered broad-spectrum include fluoroquinolones, cephalosporins, glycopeptides, penicillins, oxazolidinone, nitroimidazoles, and carbapenems.
Infections that are commonly prescribed broad-spectrum antibiotics include those affecting the bone, heart, brain, soft tissue, or skin.
A benefit of broad-spectrum antibiotics is that, by being effective against many bacterial strains, they can rid the body of the infection while also reducing the threat of hospital readmission. This makes broad-spectrum antibiotics a critical tool in the fight against hospital-acquired infections.
In addition to preventing healthcare-associated infections, broad-spectrum antibiotics can also be effective when the physician is unsure of the specific bacteria causing the infection, as broad-spectrum antibiotics can treat a wide range of bacteria. In these cases, the physician suspects a bacterial infection, but the group of bacteria is unknown, or they suspect that the infection encompasses multiple groups of bacteria.
Some antibiotics that are considered broad-spectrum include:
Broad-spectrum antibiotics, as we know, treat a broad range of bacteria, generally spanning both gram-negative and gram-positive. The alternative is narrow-spectrum antibiotics, which treat only a specific group of bacteria or a few types.
Narrow-spectrum antibiotics are just as effective as broad-spectrum antibiotics at treating infections. The primary difference is that, for them to be effective, the physician needs to be sure of the type of bacteria causing the infection to ensure that it falls within the narrow-spectrum antibiotic’s capabilities. In comparison, broad-spectrum antibiotics require less certainty regarding the type of bacteria present.
While broad-spectrum antibiotics offer many benefits, including the ease with which they can be prescribed and the greater certainty that they can treat an infection, there are also some risks associated with them.
One of the most significant risks of broad-spectrum antibiotics is antibiotic resistance, which is when the bacteria causing an infection are resistant to the antibiotic and are able to survive and keep growing. This then becomes a problem as someone believes they are taking medication to stop their infection when their infection is instead continuing to grow.
Not only does antibiotic resistance allow the infection to continue unchecked, but antibiotic-resistant bacteria are also harder to treat.
Furthermore, when it comes to infections that are resistant to drugs, it is often the broad-spectrum drugs that they have developed a resistance to, such as quinolones which have an increasing number of infections resistant to them.
When taking broad-spectrum antibiotics, it is crucial to be aware of any worsening symptoms, as this may indicate that the bacteria are resistant to the infection. Contact your physician if your symptoms do not improve or worsen after a few days of being on your antibiotic, as they may want to switch you to a different antibiotic, such as a narrow-spectrum variety.
Broad-spectrum antibiotics generally have more side effects, including rash or diarrhea. In severe cases, antibiotics may result in side effects such as C. diff infections and severe or even life-threatening allergic reactions. Compared to narrow-spectrum antibiotics, broad-spectrum antibiotics are more likely to cause these severe side effects
Research has also found that those with diabetes, in particular, are at an even greater risk of experiencing severe side effects when prescribed broad-spectrum antibiotics.
There’s yet another risk associated with broad-spectrum antibiotics, specifically for patients experiencing sepsis or whole-body infection.
A study found that broad-spectrum antibiotics are frequently prescribed to patients not infected with antibiotic-resistant bacteria and are also associated with higher mortality rates in these patients.
Conversely, undertreating a bacterial infection with an antibiotic that does not treat the bacteria is also associated with higher mortality. So, there is an ideal zone where the antibiotic treats the bacteria but is not so broad. The authors of this study use their research as proof that the application of broad-spectrum antibiotics for those who are septic needs to be more judicious.
Antibiotics are some of the most commonly prescribed medications, and they are taken in order to treat bacterial infections. There are hundreds of antibiotics, separated into classes based on their chemical structure and physiologic properties. However, they can be divided even further into two categories: broad-spectrum and narrow-spectrum.
Broad-spectrum antibiotics, as their name suggests, can treat a broad range of bacterial infections, spanning both gram-negative and gram-positive varieties. This makes them an advantageous option if a doctor suspects a bacterial infection but does not know the specific type or if they suspect an infection from multiple bacteria strains.
However, there are risks with broad-spectrum antibiotics, such as an increasing risk of antibacterial resistance and a greater risk of side effects, both mild and severe. As such, broad-spectrum antibiotics are generally not recommended if the doctor can narrow down the infection to a single strain and there is a narrow-spectrum antibiotic that can treat it.
Content on the DrHouse website is written by our medical content team and reviewed by qualified MDs, PhDs, NPs, and PharmDs. We follow strict content creation guidelines to ensure accurate medical information. However, this content is for informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment. For more information read our medical disclaimer.
Always consult with your physician or other qualified health providers about medical concerns. Never disregard professional medical advice or delay seeking it based on what you read on this website.
If you are experiencing high fever (>103F/39.4C), shortness of breath, difficulty breathing, chest pain, heart palpitations, abnormal bruising, abnormal bleeding, extreme fatigue, dizziness, new weakness or paralysis, difficulty with speech, confusion, extreme pain in any body part, or inability to remain hydrated or keep down fluids or feel you may have any other life-threatening condition, please go to the emergency department or call 911 immediately.
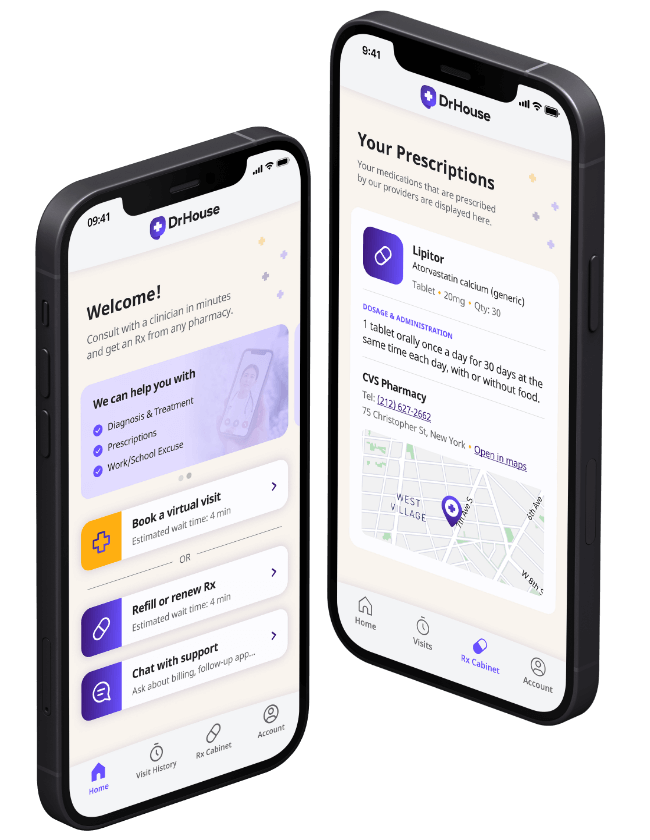
DrHouse provides 24/7 virtual urgent care, men’s health, women’s health and online prescriptions.



















Prescriptions as needed
Renew or get a new Rx.
On-demand virtual visits
See a physician 24/7.
24/7 care support
We are here to help you.
on your schedule
Skip the unnecessary waiting room, see a board-certified clinician now.